As we continue the political transition post Donald Trump’s election victory, healthcare reform and the campaign promise to Make America Healthy Again (MAHA) is making news. At the center of the MAHA movement is Robert Kennedy, Jr., an evangelist of lifestyle changes, particularly within the U.S. diet, to promote health. Kennedy openly states, and correctly so, that a major driver of U.S. healthcare costs is the declining health of the population, ripe with obesity and in turn, chronic health conditions (e.g., diabetes, high blood pressure). A bit has changed since I first wrote about “likely” Trump health policy during the campaign season https://rhislop3.com/2024/08/13/donald-trump-likely-health-policy/
I’m a data guy so it didn’t surprise me that a recent study from the Insitute of Health Metrics and Evaluation (IHME), published in the Lancet (medical journal) concluded that the U.S. life expectancy will tick-up a touch but compared to the rest of the world, by 2050, our standing as measured by life expectancy will lag nearly all other first-world countries. Increases in U.S. life expectancy forecasted to stall by 2050, poorer health expected to cause nation’s global ranking to drop | Institute for Health Metrics and Evaluation
- The U.S. is forecasted to fall in its global rankings below nearly all high-income and some middle-income countries.
- Drug use disorders, high body mass index, high blood sugar, and high blood pressure are driving mortality and disability higher across the U.S.
Researchers at the University of Washington’s Institute for Health Metrics and Evaluation in Seattle have analyzed trends for 359 diseases and injuries to project state and national life expectancy up to 2050. Life expectancy in the U.S. is expected to rise from 78.3 years in 2022 to 79.9 years in 2035, and further to 80.4 years by 2050 for all sexes. This slight increase is projected to drop the country’s global ranking from 49th in 2022 to 66th in 2050 among 204 countries and territories. The data is included in the latest Global Burden of Disease (GBD) study. Key study points are,
- The nation’s ranking for healthy life expectancy — the number of years a person can expect to live in good health — is projected to fall from 80th in 2022 to 108th by 2050.
- The increase in life expectancy is due to declining mortality rates from ischemic heart disease, stroke, cancer, and diabetes. However, deteriorating health outcomes due to obesity, high blood sugar, and drug use disorders remain significant threats. Alarmingly, drug-related mortality is expected to rise by 34% by 2050, which is the highest projected increase of any country.
- Researchers indicate that there are opportunities to alter the course of American health outcomes by enhancing healthcare access, increasing preventive care, and investing in scientific innovation, among other critical measures.
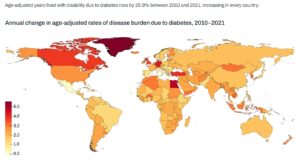
The most significant contributor to lower life expectancy and in return, quality of life years, is the rise in obesity and overweight rates. A fatter nation is a more expensive user of healthcare as obesity drives a host of other chronic diseases and requisite engagements with higher cost care (e.g., diabetes, high blood pressure, joint replacements due to being overweight, heart disease, vascular disease, etc.).
Another significant contributor to a lag in life expectancy improvement in the U.S. is the rise in drug use disorders and deaths related to criminal drug use, most recently, fentanyl. From 1990 to 2021, the U.S. experienced an increase in drug related (drug use disorder) fatalities of 878% (19.5 deaths per 100,000). This death rate is expected to increase by 34% between 2022 and 2050 (from 19.5 deaths per 100,000 to 26.7).
According to the Institute for Health Metrics and Evaluation, the elimination of major risk factors such as obesity, high blood sugar, and high blood pressure by 2050 could prevent 12.4 million deaths in the U.S. However, even if these risk factors were eradicated worldwide, the resulting health improvements would not suffice for the U.S. to advance its global health ranking, and it would continue to trail behind certain peer nations.
IHME scenarios suggest that addressing a single risk factor could save millions of lives. For instance, reducing smoking to match the lowest rates in the U.S. could result in 2.1 million fewer deaths by 2050. Similarly, if high body mass index and blood sugar levels were reduced over the same period, 1.4 million deaths could be prevented.
A recent JAMA study found that among adults with Medicare that had one or more common comorbid conditions, a 5% weight loss was estimated to reduce spending by $1,262 and a 25% weight loss was estimated to reduce spending by an average of $5,442. Estimated Reduction in Health Care Spending Associated With Weight Loss in Adults | Health Policy | JAMA Network Open | JAMA Network