In this year’s final rule (PPS) for SNFs, CMS indicated that it would delineate proposals for final rule making this spring regarding mandated staffing levels. In the 2023 Final Rule, CMS solicited comment regarding staffing level mandates. In yesterday’s post on labor and job data, I covered how incomplete the staffing picture remained for senior living in terms of widespread openings across all care facility types.
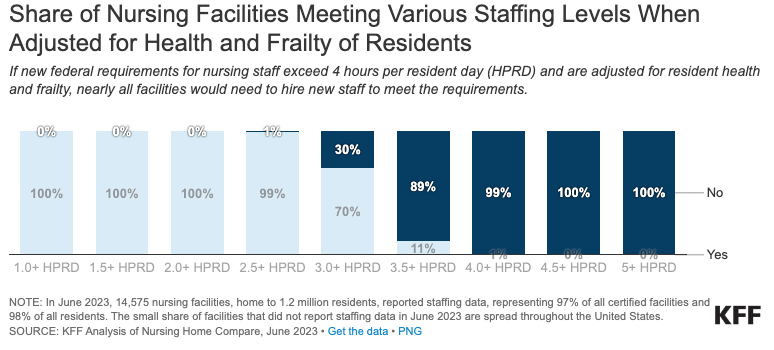
While CMS has yet to release its proposals, a recent report by the Kaiser Family Foundation (KFF) noted that only 45% of facilities could meet a 3.5 hours per patient day requirement and only 29% could meet a 4-hour standard. In Texas, only 12% of SNFs could meet a 4-hour standard. The “devil” however, is in the details in the form of what mix of staff must comprise any staffing standard (RNs, CNAs, other).
Forty-five states have existing staffing level standards with New York requiring 3.5 hours per patient day and the District of Columbia requiring 4.1 hours per patient day. New York’s requirement specifies that no less than 2.2 hours of its requirement be met by CNAs and 1.1 by RNs or LPNs.
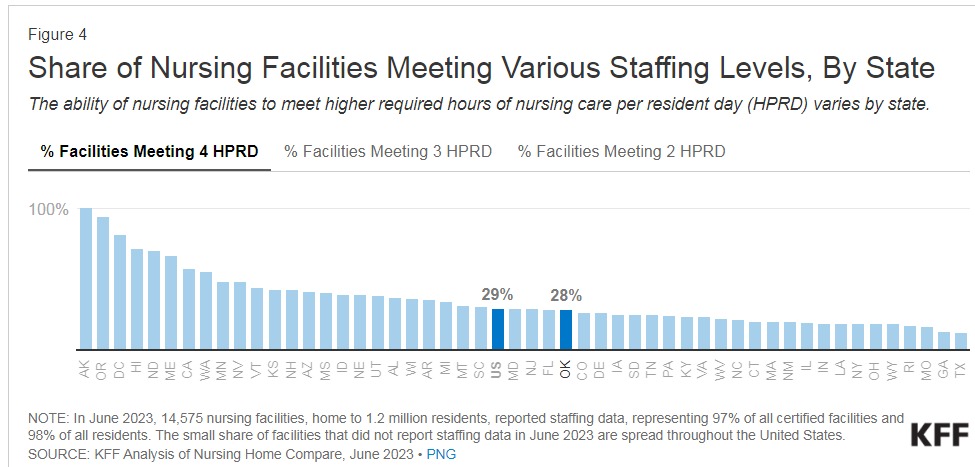
Based on current staffing levels at the vast majority of facilities, mandates that focus on increasing licensed nursing hours (RN or LPN) will be difficult to meet. If the Federal mandate also includes acuity adjustments or scales, the mandates will be even more problematic for most facilities.
Federal staffing level requirements date back to the 1987 Nursing Home Reform Act. In 2016, the Obama administration created a 3.0 hours per resident day, nursing services standard combined with a requirement for an RN to be on duty 8 hours per day, seven days per week (minimally). There is also a standard withing the Conditions of Participation (regulations to participate in the Medicare/Medicaid programs) requiring facilities to provide staffing levels “sufficient to meet the needs of their residents”. Between 2021 and 2022, 19% of facilities received citations for inadequate nursing services levels. Citations ranged from immediate jeopardy to actual harm to minimal harm (IJ, G or higher, E or. lower).
As the industry continues to wait for Federal rulemaking on a staff mandate, questions/concerns remain.
- Will the new levels be immediate or phased in?
- Will certain staff by license/certification be required (RN numbers vs. CNA numbers). A total number is easier (in theory) to comply with than staff by certain hour conditions?
- Will acuity factors be part of the requirements?
- Will other staff be part of the requirement such as therapy personnel, social workers, etc.?
- Will the level be a daily requirement or an average across a specific time period, variability allowed per census and if applicable, an average for acuity vs. daily (census and acuity fluctuations for those facilities that are predominantly post-acute focused can be profound)?
A final area to watch as staffing mandates move forward is enhanced litigation risk. The more standards become granular and perhaps, tied to acuity, the greater likelihood that negative care outcomes, even those that are not the fault of the facility specifically, will be slanted to incorporate a staffing level dimension.
The report from Kaiser is available here: https://www.kff.org/medicaid/issue-brief/what-share-of-nursing-facilities-would-meet-possible-new-staffing-requirements/#appendix