Yesterday, a story in the Washington Post highlighted a series of wandering cases where residents from an Assisted Living or Memory Care facility wandered and were later, found dead. Industry insiders knew this story was coming and yesterday, it dropped. In many ways, it is eerily similar to a PBS story a decade ago around poor care/neglect in Assisted Living facilities (life and death in Assisted Living was the title).
- The PBS Feature (video) from 2013 is here: https://www.pbs.org/video/frontline-life-and-death-assisted-living/
- The Washington Post story from yesterday is here: https://www.washingtonpost.com/business/interactive/2023/assisted-living-wander-patient-deaths/?pwapi_token=eyJ0eXAiOiJKV1QiLCJhbGciOiJIUzI1NiJ9.eyJyZWFzb24iOiJnaWZ0IiwibmJmIjoxNzAyNzg5MjAwLCJpc3MiOiJzdWJzY3JpcHRpb25zIiwiZXhwIjoxNzA0MTcxNTk5LCJpYXQiOjE3MDI3ODkyMDAsImp0aSI6IjM3Yzc5NTg5LTcwZmItNGZmZi05NTdkLTYzNmI1YzQzZjVjZiIsInVybCI6Imh0dHBzOi8vd3d3Lndhc2hpbmd0b25wb3N0LmNvbS9idXNpbmVzcy9pbnRlcmFjdGl2ZS8yMDIzL2Fzc2lzdGVkLWxpdmluZy13YW5kZXItcGF0aWVudC1kZWF0aHMvIn0.7L7VCT6CXBNxq5RRSODPYHBRigimFjK5HZIQ1Wl2VEQ&itid=gfta&utm_campaign=a91290eff6-LNK-092023_COPY_01&utm_medium=email&utm_source=LeadingAge&utm_term=0_4d92d1fd96-a91290eff6-613223933
In 2013 I wrote two posts about the PBS story and what could/should be done in the industry to reduce instances of neglect/poor care. Both posts are linked below.
- https://rhislop3.com/2013/07/29/emerituspbs-and-a-window-on-assisted-living/
- https://rhislop3.com/2013/08/06/assisted-living-pbs-and-the-lessons-learned/
Per the Washington Post story, since 2018, more than 2,000 people have wandered away from Assisted Living or Memory Care facilities or were left unattended outside, leading to 100 (approximate) deaths. Like the story, I doubt these numbers are accurate as the number of incidents that occur and go unreported are far higher.
The leading cause of death or injury is exposure (heat or cold) followed by accidents such as a fall, getting hit by a car, or drowning.
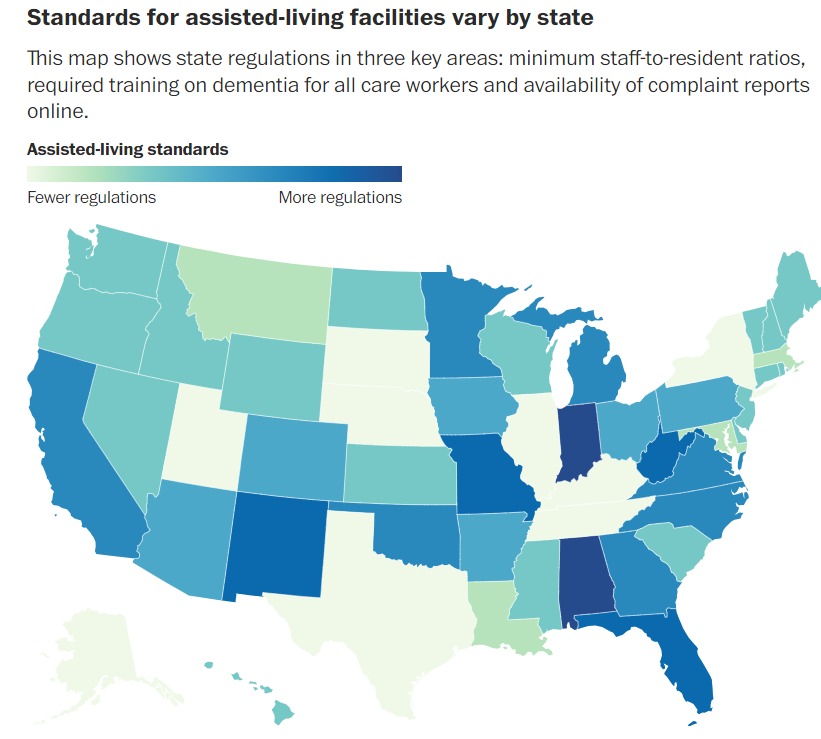
There are 30,000 plus Assisted Living and Memory Care facilities. There is no federal regulation for Assisted or Memory Care facilities, but each state does have licensing and regulatory requirements, some more stringent than others. The total number of residents in Assisted and Memory Care is approximately 1,000,000 and, growing.
The industry demand continues to be strong, principally for seniors with cognitive impairments. The next biggest segment of growth is “higher acuity” residents that formerly, would have been cared for in a nursing home. The higher acuity segment is folk that don’t necessarily require daily skilled nursing or rehabilitative therapies (PT, OT) but do have medical conditions that require skilled management services by an RN (medications, skin conditions requiring treatments, diet modifications, etc.). For families/residents that have resources (financial), the allure of a private room in a residential setting often is viewed as a far better alternative than a more institutional-style nursing home.
As has been the case since the PBS story in 2013, the primary cause of wandering, poor care, neglect, etc., is staff in number and qualification, insufficient to care for the residents in the facility. Often, the training staff receive is minimal and less tied to the condition or needs of the residents, more tied to general issues such as fire safety, resident rights, etc.
Per the Post article, only 29 states have complete and up-to-date inspection records available online. Important to note, even these reports tend to be dated as inspections for Assisted Living and Memory Care facilities are less frequent than nursing home inspections (federally mandated to be annual or within 12 to 18 months). With states having staffing problems, retaining sufficient regulatory staff to conduct annual inspections or to conduct timely follow-up on complaints or incidents, is a known challenge.
For decades, as the industry grew, increasing calls from resident rights groups and advocacy groups for federal regulatory interventions have occurred. The difficulty in gaining traction at the federal level is that the vast majority, 90% plus of Assisted and Memory care is paid for privately. The federally regulated senior living and post-acute segments receive substantial payments from Medicare and Medicaid. Prior to Medicare and Medicaid, there was virtually no regulation in SNFs and/or hospitals for that matter and what there was, was at the state level.
When regulatory infractions do occur, the remedies are typically, fairly light. Monetary penalties are the most common but rarely, do the same amount to more than a few thousand dollars. The result is a growing number of legal actions taken against providers, in an attempt to create a remedy for substandard care. The problem with litigation is that the cases take a long time, often years, to come to resolution and those bringing the suit, tend to tire and look toward settlement versus trial.
I suspect that this is not the last time issues regarding poor or substandard care in Assisted Living and Memory Care facilities will make sensational news stories. The industry is growing and residents in need of care, are as well. The challenge will be creating a system of solid, transparent performance standards. Increased regulation rarely improves the service/care delivery, as is evident in the nursing home industry. Regulation, even well intended such as staffing mandates, will have little impact if the desired standard is impossible to meet. The industry is already very expensive and ineffective regulatory policies will only raise the cost, reducing access for those that need the care but, not readily, improve the care delivered.
Leave a Reply