As of the latest demographic data from Pew Research, 62 million people in the U.S. are age 65 or older Number of people 100 and older is growing in US and around the world | Pew Research Center Presently, there are approximately 7,500 licensed geriatricians in the U.S., or 1 per every 8,267 seniors. Despite an aging population, the number of physicians specializing in geriatric medicine is not keeping pace. This should be a cause for concern.
In the last two decades, the population of Americans aged 65 and older has grown from 35 million to 58 million, and it is projected to reach 78 million by 2040. However, the U.S. healthcare system and its workforce have not scaled accordingly.

Aging comes with various health risks such as chronic diseases, overmedication, injuries from falls, and cognitive deterioration. Geriatricians play a crucial role in managing, postponing, and even averting many of these issues associated with aging. They are adept at caring for the elderly with intricate chronic conditions, prescribing safe and efficacious medications, and tackling both functional and cognitive impairments.
In the U.S. healthcare system today, 90% of the $4.5 trillion annual expenditure goes toward treating chronic medical and mental illnesses (the preponderance to medical conditions) Fast Facts: Health and Economic Costs of Chronic Conditions | Chronic Disease | CDC For example,
- More than 38 million Americans have diabetes, and another 98 million adults in the United States have prediabetes, which puts them at risk for Type II diabetes. Diabetes can cause serious complications, including heart disease, kidney failure, and blindness. In 2022, the total estimated cost of diagnosed diabetes was $413 billion in medical costs and lost productivity. The percentage of adults with Type II diabetes rises significantly with age, to 29.2% of adults 65 and older.
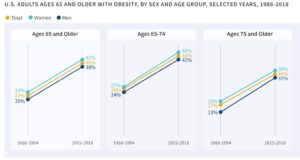
- Obesity impacts 20% of children and 42% of adults, posing a risk for chronic conditions like type 2 diabetes, heart disease, and certain cancers. Slightly more than one-third of young adults between 17 to 24 years old are overweight to the extent that they are ineligible for U.S. military service. Obesity incurs an approximate annual cost of $173 billion to the U.S. healthcare system. Obesity rates among older adults have doubled in a generation.
- Alzheimer’s disease, a form of dementia, is an incurable, progressive brain disorder that impacts close to 7 million Americans, including one out of every nine adults over the age of 65. Among these older individuals, women constitute two-thirds (4.2 million). Alzheimer’s disease-related deaths have more than doubled from 2000 to 2021, rising by 141%. The expenses associated with caring for individuals with Alzheimer’s and other dementias are estimated at $360 billion in 2024, with projections nearing $1 trillion (in current dollars) by 2050.
- Arthritis affects 53.2 million adults in the United States, which is about 1 in 5 adults. It is a leading cause of disability in the United States, and a leading cause of chronic pain. Arthritis-attributable medical costs and earning losses were over $300 billion in 2013. Arthritis increased with increasing age, from 3.6% in adults ages 18–34 to 53.9% in those age 75 and older.

While this post is about the need for more Geriatricians (doctors specializing in the care of older adults), the reason for the importance of this situation is our aging population. Aging populations have profound impacts on their respective societies, economically and socially in terms of social supports, disability, and healthcare utilization. See a post I wrote earlier this year on this subject https://rhislop3.com/2024/01/04/__trashed/
Despite the obvious need due to demographic trends, the number of healthcare professionals trained and experienced in geriatric care is on the decline. An increasing number of medical students and residents are opting out of becoming geriatricians. For instance, in 2023, only 174 out of 419 available positions in geriatrics fellowship training were filled through the national specialty match, marking the lowest fill-rate among all medical specialties. This waning interest in geriatrics extends to other healthcare professions, including nurse practitioners. While there are nearly 400,000 licensed nurse practitioners in the U.S., crucial in various healthcare settings, the specialization as a geriatric nurse practitioner ceased to be an option approximately a decade ago due to lack of interest.
Financial rewards, prestige, and respect significantly impact the appeal of medical specialties to students, residents, and nurse practitioners. Specialties such as cardiology, oncology, and dermatology are notably more profitable than geriatrics, ensuring their training programs consistently attract applicants.
All medical students must undergo clinical training in pediatrics and obstetrics, despite the fact that many will not treat children or deliver babies after graduation. However, with the shifting demographic landscape, the care of older adults will comprise a growing segment of health care providers’ workloads in the years ahead. Paradoxically, as noted at the 2024 annual meeting of the American Geriatrics Society, just one in ten U.S. traditional and osteopathic medical schools require a clinical rotation in geriatrics, down from one in four in 2010. 2024 Abstract Supplement
In the 2000s, I was the CEO of an older adult, senior living system – one of the largest in the country. We had as part of our system, medical clinics with employed physicians, board certified in geriatrics. Knowing the demographic shift and seeing the decline in physicians embracing geriatrics along with the lack of geriatric training as part of medical education, we began a geriatric rotation program for all medical students (family practice) at the Medical College of Wisconsin. Simultaneous, we developed and integrated a dental residence program and geriatric rotation with Marquette University’s School of Dentistry (we had a dental clinic as part of our integrated medical/outpatient care programs).
I left the system in 2009 to form my own business and lacking champions/commitment from the Medical College and Marquette, the programs slowly died. To me, this was tragic as the field for innovation and continued development was wide open.
The United States is only starting to feel the full effects of its aging population. Unfortunately, the healthcare system and workforce are not sufficiently prepared to manage the impending increase in multimorbidity, dementia, functional impairment, and frailty. Leaders of healthcare organizations and medical schools have either not acknowledged this issue or, even worse, chosen to ignore it. Geriatrician shortage looms as baby boomers age | STAT (statnews.com)