The Senate has approved a spending bill to keep the federal government running through January 30, though any decisions about extending the ACA enhanced premium tax credits have been postponed until December.
Here are the main highlights:
- The package, passed with a 60-40 vote, will fund the Department of Agriculture, Food and Drug Administration, and Department of Veterans Affairs for the entire fiscal year, while other departments like HHS will be funded only until the end of January.
- Under the agreement, the Senate can vote in December on legislation to prolong the enhanced ACA subsidies, which are scheduled to expire at the close of 2025. It also includes provisions for retroactive pay to federal employees and reverses layoffs from the shutdown.
- The bill headed to the House of Representatives today, where a vote could occur at any time.
- According to InsideHealthPolicy.com | An Inside Washington news service, the deal will likely reimburse healthcare providers for unpaid Medicare telehealth visits during the stoppage, with telehealth claims paid retroactively from October 1. Claims that were previously reimbursed at lower rates due to geographic rule changes would probably be reprocessed.
- The agreement extends funding for the Supplemental Nutrition Assistance Program (SNAP) through fiscal 2026. SNAP benefits expired on November 1, and ongoing legal disputes have affected short-term funding. On November 9, a federal appeals court denied the Trump administration’s attempt to prevent full funding of the program for November, as ordered by a circuit judge (the government must issue payments within 48 hours unless halted by the Supreme Court). With a potential end to the government shutdown in sight, the Supreme Court on Tuesday extended a freeze on a federal judge’s ruling that would require the Trump administration to fully fund the SNAP food program in November.
One of the major challenges embedded within the ACA subsidy issue is a concern about fraud or fraudulent enrollment. Since COVID era expansion, there has been a growing series of voices raising alarm (I am one) that the enrollment growth seemed juxtaposed to known utilization trends. The graph below, courtesy of the Competitive Enterprise Institute illustrates a gap between surveyed brokers and participants and CMS data.
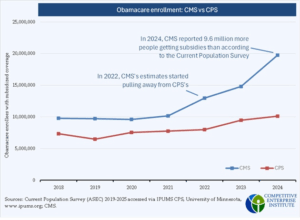
There is speculation that significant improper enrollment may result in a higher proportion of enrollees who do not utilize their health plans. According to research, this trend has been observed: 35% of all enrollees and 40% of fully subsidized enrollees did not use their health plan at any point during their enrollment period. Further analysis separating full-year enrollees from partial-year enrollees would be valuable; however, CMS does not have the capability to provide data at this level of detail. Research and file courtesy of the Paragon Health Institute Obamacare-Fraud-by-the-Numbers-RELEASE_V3_251112_154210
What comes next based on the House vote today, to end the government shutdown (and to revisit ACA subsidies set to expire) is as follows.
- Shutdown Resolution: A bipartisan agreement reopened the government, postponing subsidy decisions to December. House Democrats tried but failed to secure 3-year extensions.
- Democrats favor a clean 1-3 year extension at an estimated cost of $350 billion through 2035, with Minority Leader Jeffries labelling the situation a “Republican healthcare crisis.”
- Republicans oppose additional spending and seek reforms such as annual eligibility checks, ending silver loading, and abortion restrictions. Senate Republicans continue discussions on measures like lowering income caps.
President Trump proposed sending $115 billion in subsidies directly to individuals via Health Savings Accounts, bypassing insurers, which critics warn could destabilize ACA insurance pools. The Senate floor vote promised post-shutdown, a vote on subsidy continuation (COVID era), set to expire on 12/31/25. A Bipartisan deal is possible for a 1-year extension (~$100B), but Trump’s direct-payment push and GOP reforms (e.g., fraud curbs via Trump-era rules) complicate it. Failure to extend the subsidies means 2026 hikes hit January 1.
For readers interested in a more detailed history of Medicaid spending reduction/reform proposals that are part of the Trump healthcare agenda, a good link to articles on this site is here: https://rhislop3.com/republican-house-medicaid-reform-package/
1 thought on “Congress, Medicaid Subsidies – What’s Next”