The Centers for Medicare & Medicaid Innovation (Innovation Center), formerly known as CMMI and part of the Centers for Medicare & Medicaid Services (CMS) under the US Department of Health & Human Services (HHS), has released a White Paper (CMS Innovation Center Strategy to Make America Healthy Again | CMS ) outlining a strategic direction for 2025 and beyond. The paper emphasizes a commitment to value-based care by using lessons from the past 15 years to enhance healthcare delivery through three strategic pillars: promoting evidence-based prevention, empowering beneficiaries, and expanding choice and competition.
Promote Evidence-Based Prevention
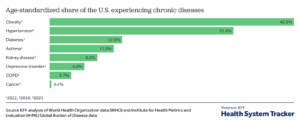
The Innovation Center will embed preventive care in every model, emphasizing primary, secondary, and tertiary prevention. This includes incentivizing healthier lifestyles through physical activity, nutrition counseling, and access to evidence-based complementary and alternative medicine. The goal is to delay or prevent chronic diseases, which affect 60% of Americans, reducing costly treatments and saving taxpayer dollars. Models will measure outcomes to ensure effectiveness.
- Heart disease and stroke: $254 billion in healthcare costs and $168 billion in lost productivity.
- Diabetes: $413 billion in medical costs and lost productivity in 2022.
- Obesity: $173 billion in healthcare costs.
- Arthritis: Over $300 billion in medical costs and lost earnings (2013 data).
- Epilepsy: $13.4 billion in total healthcare costs in 2019.
- Physical inactivity: $117 billion in related healthcare costs.
Empower People to Achieve Health Goals
The strategy prioritizes giving patients better access to health data and tools, such as mobile apps, to manage diseases and make informed decisions. Building on initiatives like Blue Button, the Innovation Center aims to enhance data transparency and align financial incentives to support patient-provider collaboration, reducing out-of-pocket costs and improving outcomes.
This strategy follows closely with other initiatives CMS has played with in regard to interoperability. The Hitech Act and HIPAA included various pieces. In 2018, I wrote a post on interoperability in post-acute care. That post is available here: https://rhislop3.com/interoperability-and-post-acute-implications/
- The goal is to empower patients with control over their health data, facilitating better decision-making, care coordination, and engagement with providers.
- The initiative has evolved to include private sector partners and supports formats like PDF, text, or structured data (e.g., FHIR standards). It’s part of broader efforts, like those under the CMS Innovation Center, to enhance data transparency and interoperability, aligning with policies such as the 21st Century Cures Act. As of 2025, Blue Button 2.0, an API-based version, enables developers to create apps that integrate Medicare claims data, serving over 60 million beneficiaries.
Drive Choice and Competition
The Innovation Center will foster competition by expanding provider participation, especially for independent and rural practices, and supporting patient choice in care settings, including at-home care. Models will require downside risk, meaning providers share financial losses if costs exceed targets, and reduce reliance on state rate-setting. This aims to lower costs through market-driven efficiencies while prioritizing high-value care.
The strategy also emphasizes at-home care, with potential expansions like hospital-at-home or skilled nursing facility-at-home models, though details remain forthcoming. Existing models, such as the Home Health Value-Based Purchasing Model, are likely to continue with savings of $141 million annually. However, eight payment models, including Making Care Primary and End-Stage Renal Disease Treatment Choices, will be terminated by year-end to focus on those meeting statutory cost-saving and quality goals.
An element that is not specifically addressed but has been bandied about within value-based care models is site neutral payments. I wrote a post on site neutral payments in post-acute care back in 2018. The post is here: https://rhislop3.com/post-acute-site-neutral-payment-upcoming/
- Hospital Outpatient Department: (approx) $1,200 (OPPS rate).
- Ambulatory Surgery Center: (approx) $600 (ASC payment system).
- Physician Office: (approx) $400 (physician fee schedule). Site-neutral payments would standardize reimbursement, potentially at the lower ASC or office rate, reducing costs without affecting care quality.
- Current Issue: Medicare payment rates vary by site. For example, in 2023, HOPDs were paid $201 for a Level 2 E/M visit (CPT 99212-99215), while physician offices received $108 for the same service. This discrepancy drives higher costs, as hospitals acquire physician practices, shifting care to HOPDs.
- Policy Implementation: The Bipartisan Budget Act of 2015 (Section 603) initiated site-neutral payments for certain off-campus HOPDs, paying them at physician fee schedule rates instead of higher outpatient prospective payment system (OPPS) rates. In 2019, CMS expanded this to clinic visits (HCPCS code G0463), applying site-neutral rates to all off-campus HOPDs, saving an estimated $610 million annually.
- Impact: Site-neutral policies aim to reduce Medicare spending (projected to exceed $1 trillion by 2028) and beneficiary cost-sharing, as higher HOPD rates increase coinsurance. They also encourage competition by leveling the playing field for independent practices and ASCs.
- Challenges: Hospitals oppose these policies, arguing they face higher regulatory and operational costs. Critics claim site-neutral payments could limit access to care, especially in rural areas, though evidence suggests minimal impact on patient access.
- Recent Developments: The CMS Innovation Center’s 2025 strategy emphasizes competition and cost reduction, potentially expanding site-neutral policies to align with the “Make America Healthy Again” initiative. The Trump administration has prioritized these reforms to curb hospital consolidation and lower costs.
This approach aims to address unsustainable healthcare costs, with Medicaid as a top state expense and Medicare’s Trust Fund projected to be insolvent by 2036. By prioritizing prevention and value-based care, the Innovation Center seeks to reduce wasteful spending and improve health outcomes, aligning with MAHA’s vision. More details on new models are expected in the coming months.