Medicaid potential spending cuts have been in the news, elevated by the passage of the recent Republican Continuing (spending) Resolution. As Donald Trump ran and got elected on a platform of spending reduction/debt reduction (austerity) including the activation of DOGE (Dept. of Government Efficiency) to identify spending reduction opportunities, program behemoths like Medicare and Medicaid come front-and-center in savings discussions. More on Medicaid and DOGE is here: https://rhislop3.com/medicaid-spending-in-the-doge-radar/
To frame the discussions on Medicaid reforms and potential spending reductions, I’ve done some fairly deep analysis into the proposals and discussions emanating from Washington. This post is Part I of likely a two-part, perhaps three-part, series on Medicaid, possible reductions, program changes, etc.
Analyzing Proposed Spending Cuts to the Medicaid Program in 2025
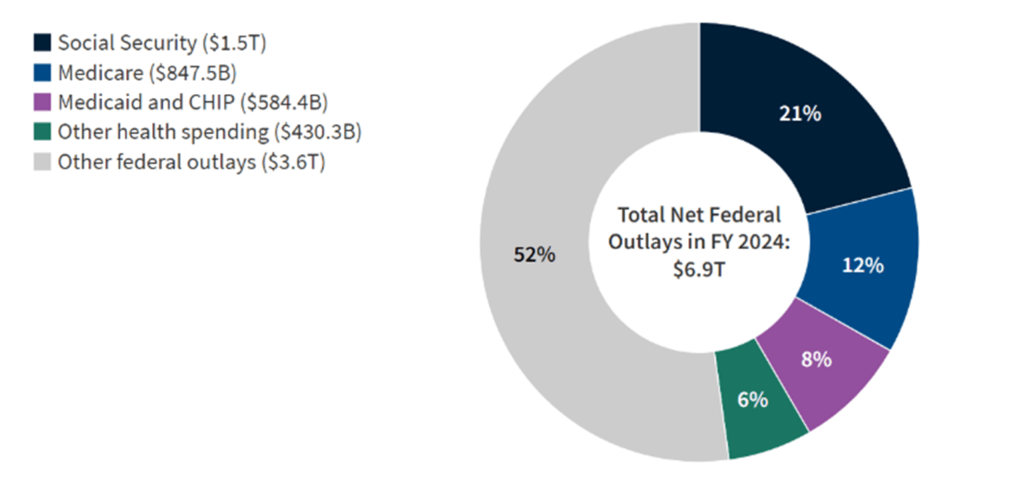
The Medicaid program, a safety net providing health coverage to over 90 million low-income Americans, is facing significant potential spending cuts as part of ongoing budget negotiations in Congress. These proposed reductions, which could reshape the program’s structure and accessibility, are being considered as part of broader efforts to address federal spending and a $36 trillion (and growing) debt burden. Medicaid, which accounts for nearly one-fifth of all U.S. healthcare expenditures, has become a focal point for policymakers seeking to reduce the federal deficit and bring the budget into balance (not adding additional debt levels to the current debt total).
Currently, the federal government covers 90% of the costs for Medicaid expansion enrollees in the 41 states (including Washington, D.C.) that have opted into the ACA expansion. However, proposed changes by House Republicans could alter this funding model by imposing per capita spending caps, work requirements and reducing the enhanced Federal Medical Assistance Percentage from 90% to each state’s standard Medicaid matching rate, which varies between 50% and 74%.
Among the most prominent proposals is a plan to cut $880 billion from Medicaid over the next decade, as outlined in the House Budget 2025 bill. These cuts would likely involve measures such as implementing per-capita caps, reducing the federal match rate for Medicaid expansion under the Affordable Care Act (ACA), and introducing work requirements for certain beneficiaries. Proponents argue that these changes would curb program growth and encourage fiscal responsibility, while critics warn of devastating consequences for vulnerable populations, including low-income families, children, seniors, and individuals with disabilities.
Federal Budget Resolution and Medicaid Reductions
The House of Representatives recently passed a budget resolution (H Con Res 14, 119th Congress) proposing $880 billion in Medicaid cuts over the next decade. This measure is part of a broader Republican-led initiative aimed at reducing the federal deficit while extending $4.5 trillion in tax cuts (current tax rates from the TCJA). Medicaid, which currently provides health coverage to nearly 80 million Americans, would face significant funding reductions if the resolution becomes law. The cuts would constitute approximately 11% of the federal government’s projected $8.2 trillion Medicaid expenditure over the next ten years (AJMC).
The resolution directs the House Energy and Commerce Committee to identify cost-saving measures, with Medicaid being a primary target. Some analysts such as those from the Committee for a Responsible Federal Budget (CRFB), have noted that achieving the $880 billion target without substantial Medicaid reductions would be nearly impossible. Other programs overseen by the committee, such as the Children’s Health Insurance Program (CHIP), account for only $600 billion in potential cuts, leaving Medicaid as the primary source for deficit reduction.
Impact on Medicaid Expansion and Federal Match Rates
One of the proposed changes involves eliminating the 90% federal match rate for Medicaid expansion under the Affordable Care Act (ACA). This match rate currently supports coverage for over 20 million individuals. If this proposal is implemented, states would face two scenarios: either absorb the financial burden of maintaining expansion coverage or discontinue the program altogether.
Scenario 1: States Maintain Expansion Coverage
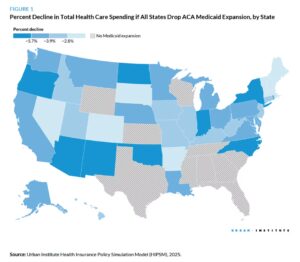
States that choose to sustain Medicaid expansion would experience a 10% reduction in federal Medicaid spending, amounting to $626 billion over a decade. Concurrently, state Medicaid spending would rise by 17% to offset the federal shortfall (KFF).
Scenario 2: States Drop Expansion Coverage
States opting to end Medicaid expansion would see a 25% decrease in federal Medicaid spending, equating to $1.7 trillion over ten years. This would result in nearly 20 million individuals losing coverage, reducing total Medicaid spending by one-fifth (KFF).
State-Level Implications
Medicaid is jointly funded by the federal government and states, meaning federal spending cuts would shift a significant financial burden to state governments. States would need to explore various strategies to manage the shortfall, including:
- Increasing State Funding: States could raise taxes or reallocate funds from other budget priorities to maintain Medicaid programs. However, this approach may face political and economic challenges (Grantmakers In Health).
- Reducing Eligibility or Benefits: States may tighten eligibility criteria or eliminate optional benefits, disproportionately impacting vulnerable populations such as children, seniors, and individuals with disabilities (AJMC).
- Block Grants: Some proposals suggest transitioning Medicaid to a block grant model, providing states with fixed funding. While this approach offers greater flexibility, it could lead to funding shortfalls during economic downturns or public health emergencies.
Legislative and Political Challenges
The proposed Medicaid cuts have sparked significant political debate. While the House narrowly passed the budget resolution in a 217-215 vote, the measure faces resistance in the Senate. Some Republican senators have expressed concerns about the depth of the cuts, while others argue for even more aggressive reductions (AJMC).
Public opinion may also play a critical role in shaping the outcome of the proposed cuts. Polls consistently show that a majority of Americans, including Republicans, support Medicaid and oppose significant reductions to the program.
More on the overall healthcare implications and economic and social considerations/concerns, in Part II.
1 thought on “Medicaid Spending Reductions: What to Know”