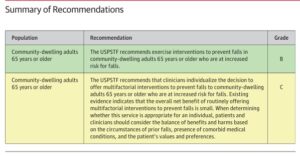
Earlier this week, JAMA (Journal of American Medical Association) published a summary article on interventions to prevent/reduce falls in community-based (non-institutionalized) seniors. The core focus of the article is about preventing falls in seniors. The article is available here: jama fall prevention in older adullts
As regular readers know, I don’t write a great deal on clinical topics, confessing my non-clinical background. From time to time however, I will run across information that I think is interesting and, easy enough to follow or digest, for non-clinical readers/followers.
Per the JAMA article, “Falls are the leading cause of injury-related morbidity and mortality among older adults in the US. In 2018, 27.5% of community-dwelling adults 65 years or older reported at least 1 fall in the past year and 10.2% reported a fall-related injury. In2021, an estimated 38,742 deaths resulted from fall-related injuries.“
Not surprising, falls are also the leading cause of decline (physical and cognitive) in institutionalized seniors and even greater in number and probability, according to the National Institutes of Health. “Falls in the elderly population are an emerging public
health problem, with clear challenges for health policies oriented to this age group. The prevalence of these events may vary according to context, but the consensus is that rates are higher in long-stay institutions for elderly people, with an estimated incidence of between 34% and 67%. Researchers have attributed this higher rate among institutionalized elderly people to increased levels of dependence, higher numbers of chronic diseases, poly-medication lack of physical activity, and greater interactions between intrinsic and extrinsic risk factors.” The full article from the NIH is available here: NIH Falls in Institutionalized Elderly
The primary fall prevention intervention recommended via the JAMA article was exercise. Secondary interventions of vitamin D and calcium supplementation correlate less to fall prevention but more so to improving bone density, especially in post-menopausal women (e.g., fracture reduction/mitigation).
From my experience, some nearly four decades worth, fall prevention, community or institutional based, requires a four pronged approach – all interventions.
- Activity and exercise focused as much as possible on balance improvement. This includes gait and core.
- Poly-pharmacy reduction and blood pressure management. Too often, falls are tied to a senior becoming orthostatic on rising. Too many medications with interactions can cause lightheadedness, fatigue, vision impairment, judgement impairment, etc.
- Minimizing environmental risks such as clutter, loose or slick surfaces (throw rugs), congestion, improper height toilets, lack of grab bars in shower/tub areas, etc.
- Proper nutrition and hydration that focuses on adequate fluid intake (minimizes orthostatic hypotension) and balanced protein and carbohydrate intake (adequacy for muscle maintenance).
Finally, for providers, take note. My firm’s compliance practice experiences fall related litigation as the highest litigation risk providers face. Anything a provider can do to minimize falls is a step toward lowering litigation risk. In Assisted Livings and now, Independent Living, increased acuity among residents presents some new challenges in terms of risk. I can’t recommend enough that as resident acuity increases, providers take appropriate and measured steps to improve staff competency, numbers if necessary, and add additional interventions to minimize risks associated with falls, poor care outcomes (skin breakdown), infections, unnecessary hospitalizations, etc.
TGIF!