Introduction
Mr. Musk’s DOGE team has requested access to CMS systems, which manage over $1 trillion in annual payments, according to documents obtained by the New York Times. This initiative, led by Mr. Musk’s longtime associate Steve Davis, aligns with a broader effort to reduce federal spending by scrutinizing payments and contracts. Hospital and health system leaders are closely monitoring potential changes to Medicaid funding, citing concerns about financial stability and patient access.
Federal Deficit and Improper Payments
The federal deficit in fiscal 2024 was $1.8 trillion, with $236 billion in improper payments in fiscal 2023, as reported by the Government Accountability Office. This amount reflects a decrease of approximately $11 billion from the previous fiscal year. The implications of these financial figures are significant, especially for healthcare providers who may face financial instability if DOGE imposes abrupt funding changes. The GAO report is here: Medicare and Medicaid: Additional Actions Needed to Enhance Program Integrity and Save Billions | U.S. GAO
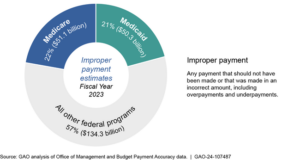
Given the current fiscal environment, it is imperative to address improper payments and ensure oversight of program spending. Over the past decade, federal spending for Medicare and Medicaid has nearly doubled, with continued growth expected.

Potential Impact on Healthcare Providers
Healthcare providers, particularly hospitals, nursing homes, and health systems dependent on Medicaid reimbursements, could experience financial instability if there are sudden changes to Medicaid funding. As the administration advances with these changes, healthcare executives must prepare for potential policy shifts that could impact payment structures, contract negotiations, and long-term financial planning.
Proposals by Republican Lawmakers
Republican lawmakers have previously suggested implementing per-capita spending caps or block grants, which would limit federal Medicaid funding and shift more costs to states over time. The Congressional Budget Office estimated that such changes could reduce federal Medicaid spending by $900 billion over the next decade, potentially causing states to cut eligibility, reduce benefits, or raise taxes.
Other Potential Medicaid Changes
Several other potential changes to Medicaid could further impact healthcare providers and patients:
- Stricter Enrollment and Renewal Requirements: Making it more difficult for currently eligible individuals to maintain coverage. During COVID, Medicaid eligibility was expanded and re-certification (annual) requirements waived. States have returned, as required by federal law, to eligibility testing. More on Medicaid qualification challenges at https://rhislop3.com/medicaid-hcbs-and-eligibility-updates/
- Elimination of Provider Taxes: Many states use these taxes, commonly known as bed taxes on inpatient provider licensed beds, to help finance Medicaid via matched federal dollars
- Potential Work Requirements: These requirements could lead to coverage losses among low-income adults or alternatively, move current Medicaid beneficiaries into ACA plans.
Conclusion
The request for CMS systems access by Mr. Musk’s DOGE team and the potential changes to Medicaid funding present significant realignment challenges for healthcare providers. Hospital, nursing home, and health system leaders, along with their trade associations, must stay informed and prepared for possible policy shifts that could affect their financial/revenue outlooks and patient care services for certain population segments. As these discussions continue, it is important for all stakeholders to engage in dialogue and advocacy to ensure that the needs of patients and providers are adequately addressed.