Potential Impacts of Medicaid Cuts on Beneficiaries and Providers
This is Part II of a series I researched and produced on Medicaid cuts. The third, which I will edit and post later in the week, will wrap it up. With healthcare spending a major economic issue, I hope these few posts provided context for readers as the debate expands. Part I is available here: https://rhislop3.com/medicaid-spending-reductions-what-to-know/
Disenrollment Due to Work Requirements and Administrative Barriers
Proposed Medicaid work requirements and increased administrative hurdles could lead to significant disenrollment among eligible beneficiaries. Work requirements, which mandate beneficiaries to prove employment or job-seeking activities, could result in coverage losses, even among those who meet the requirements. For example, Arkansas implemented work requirements in 2018, leading to over 18,000 individuals losing coverage within months due to reporting challenges rather than non-compliance (KFF).
Administrative barriers, such as stricter documentation requirements for eligibility, could further compound coverage losses. Studies show that even minor administrative complexities can deter low-income individuals from completing enrollment or renewal processes. This is particularly concerning for populations with limited access to technology or language barriers (Grantmakers In Health).
Impact on Long-Term Care Services
Medicaid is the largest payer for long-term care services in the United States, covering 42% of all long-term care expenditures, including nursing home care and home- and community-based services (HCBS). Proposed funding cuts could possibly impact older adults and individuals with disabilities who rely on these services. States could resort to reducing HCBS funding, tighten eligibility criteria, or impose waiting lists, leaving some challenges for care access. Even now, HCBS waiver slots are limited and insufficient to meet all current demand. https://rhislop3.com/medicaid-hcbs-and-eligibility-updates/
For example, a reduction in federal funding through mechanisms like per capita caps could disproportionately affect states with higher long-term care needs. States with aging populations, such as Florida and Pennsylvania, could face increased financial pressure to scale back services, raise or fund additional dollars, or shift costs to beneficiaries (National Law Review).
Provider Financial Strain and Service Reductions
Medicaid providers, including safety-net hospitals, nursing homes, and home care agencies, are likely to face at least some initial financial strain under proposed funding cuts. The question that begs is whether states will rework their Medicaid plans and formulas to maintain current reimbursement levels. Medicaid reimbursement rates are already lower than those of Medicare and private insurance, and further reductions could make it unsustainable for providers to continue serving Medicaid patients (Sheppard Healthcare Law).
Safety-net hospitals, which serve a high percentage of low-income and uninsured patients, could see reductions in disproportionate share hospital (DSH) payments. These payments are critical for offsetting uncompensated care costs. A reduction in DSH funding could destabilize these facilities, leading to closures in rural and underserved areas, already struggling to maintain providers.
Increased Uninsured Rates and Health Disparities
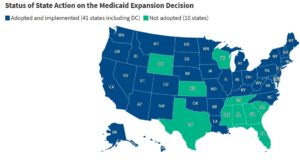
Cuts to Medicaid funding could result in millions of individuals losing coverage, increasing the uninsured rate. A per capita cap, for instance, could lead to 15 million enrollees losing coverage by 2034, with that number doubling to 30 million if combined with the elimination of the Affordable Care Act (ACA) expansion match rate. This is the funding that states received to expand their Medicaid programs – 90% funded by the Federal government.
The loss of Medicaid coverage could disproportionately affect racial and ethnic minorities, who are overrepresented among Medicaid enrollees. Hispanic and Black populations, in particular, could experience care access challenges for preventive care, chronic disease management, and maternal health services. It should be noted however, that in rural environments and inner-city environments, care access currently is a challenge for racial and ethnic communities.
State-Level Responses and Their Implications
States could face difficult choices in responding to federal Medicaid funding cuts. While some states may attempt to fill funding gaps through increased state spending, others may opt to reduce eligibility, benefits, or provider payments. For example:
- Eligibility Reductions: States could tighten income thresholds or eliminate coverage for certain groups, such as low-income adults without children. This would disproportionately impact populations in non-expansion states, where Medicaid eligibility is more restrictive.
- Benefit Reductions: Optional benefits, such as dental, vision, and mental health services, could be cut to manage budget shortfalls. This would leave beneficiaries with fewer covered services and higher out-of-pocket costs.
- Provider Payment Cuts: Lower reimbursement rates could discourage providers from participating in Medicaid, further limiting access to care for enrollees. Rural areas, which already face provider shortages, would be particularly affected (Sheppard Healthcare Law).
Economic Ripple Effects
Medicaid cuts could have broader economic implications beyond healthcare. Medicaid accounts for nearly $1 out of every $5 spent on healthcare in the U.S., making it a critical component of the healthcare economy. Reductions in Medicaid spending could lead to job losses in the healthcare sector, particularly among providers heavily reliant on Medicaid funding. The losses, however, are likely temporary as demand for healthcare workers continues to outpace supply.
Additionally, states that rely on provider taxes and intergovernmental transfers to fund Medicaid could face budgetary challenges if federal restrictions are imposed on these financing mechanisms. Without alternative revenue sources, states could struggle to maintain Medicaid programs, exacerbating economic disparities between states.
Part Three Upcoming
In the third, and final post, I’ll review the policy options that exist or have been discussed, as alternatives to cuts. As I have written many, many times, programs like Medicare and Medicaid need reform, wholesale reform. Cuts are but a blunt instrument that will do little economically over time but have social fall out that could be avoided with programmatic changes.