Within the last few weeks, I’ve had the opportunity to discuss and review, the ongoing Medicare TPE program with a number of hospices and hospice folks. Suffice to say, there are more than a few questions and resultant (still) confusion over the audit process and claims denial in general. I hope this post provides some clarity. Feel free to contact me with questions at rhislop@h2healthllc.com.
What is TPE
TPE, implemented nationwide in 2017, consists of up to three rounds of 20-40 claim reviews per provider, accompanied by targeted education initiatives intended to reduce errors. Providers selected for TPE typically demonstrate high denial rates (often exceeding 50%, depending on the service type) or exhibit outlier billing practices. In fiscal year 2019, the most recent period with comprehensive CMS-wide TPE data, approximately 13,500 providers across all categories underwent review. Of the roughly 435,000 claims assessed, about 60% were accepted as billed, and fewer than 2% of providers failed all rounds. Nearly 90,000 educational sessions were conducted, contributing to an overall reduction in appeals.
Regarding Hospice Improper Payment Rates (CERT Data), the CERT program conducts annual claim sampling to estimate improper payments, directly influencing TPE selection criteria. Improper payment rates for hospice providers increased in recent years, partly attributable to post-COVID shifts in billing practices; however, these rates stabilized in 2024. Key statistics include:
| Year | Improper Payment Rate | Projected Improper Payments | Primary Error Categories (% of Errors) | Claims Reviewed |
| 2023 | ~8.5% (estimated from prior trends; exact not isolated) | $1.3 billion | Insufficient documentation (65%), medical necessity (16%), no documentation (~15%) | Not specified |
| 2024 | 7.1% (95% CI: 4.9–9.3%) | $1.8 billion | Insufficient documentation (65.1%), medical necessity (16.3%), no documentation (14.6%), incorrect coding (1.5%) | 897 |
- Top Root Causes (2024 Sample): Inadequate/missing physician certification (29 cases), missing service intensity add-on documentation (17 cases), and missing face-to-face encounter docs (7 cases).
- These rates contribute to ~5.6% of overall Medicare Part A improper payments (excluding hospitals). TPE aims to address these via education, but CERT doesn’t track TPE-specific impacts.
Upon selection for Targeted Probe and Educate (TPE), hospices will begin receiving Additional Documentation Requests (ADRs) for claims meeting specific criteria. Each round involves a minimum of 20 and a maximum of 40 claim requests. Once ADRs are identified and documentation is submitted, the Medicare Administrative Contractor (MAC) has 30 days to review and provide feedback.
At the conclusion of each TPE round, hospices receive a results letter outlining the denial percentage, which determines progression to subsequent rounds. To avoid advancement, hospices must maintain an error percentage below the threshold established by the MAC—CGS 25%, NGS 15%, Palmetto GBA 20%. Certain triggers include length of stay exceeding 730 days with non-cancer diagnoses, Q-Codes on claims for hospice services in nursing facilities (Q5003 & Q5004), and new providers submitting at least 50 claims.
Should a hospice fail two consecutive rounds and also the third, it will be referred to CMS for further action. The decision letter provides instructions for scheduling an educational call to address denial reasons. A new TPE round, if necessary, commences 45–56 days after the call, allowing time for corrective measures.
Denials and Why
While the Centers for Medicare & Medicaid Services (CMS) do not publish comprehensive, hospice-specific national aggregate data on TPE outcomes, available insights derive from the Comprehensive Error Rate Testing (CERT) program and industry surveys such as the 2023 National Hospice Audit Survey by the Alliance for Care at Home. These resources shed light on audit burden, denial trends, and appeal outcomes, though general program effectiveness is reported in CMS literature and not disaggregated for hospice claims. A quick fact sheet on denials is here: hospice_5fftf_factsheet
Notably, the 2023 National Hospice Audit Survey, surveying 87 U.S. hospices (~10% response rate), provides focused TPE-related data for 2018–2023. Key findings include:
- Audit Prevalence: 77% of respondents underwent TPE audits in the past five years; 53% experienced multiple audit types within six months, and 31% resubmitted charts.
- Duration and Burden: 32% of TPE audits extended 18–24 months due to General Inpatient (GIP) reviews. Half considered documentation requests “extremely burdensome,” requiring additional staff. Overlaps between SMRC and TPE audits contributed to higher workload.
- Denial Rates and Reasons: Common denial codes included:
- 5PM01 (terminal prognosis unsupported): 55%
- 5PX06 (invalid election notice): 44%
- 5PM02 (GIP not reasonable/necessary): 30%
- 5PC08 (face-to-face requirements unmet): 26%
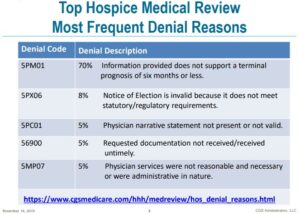
Source for the table is here: Hospice Medical Review Denials
Issues involved reviewer discretion overruling physician certifications, same-day visit denials despite proper notes, and regulatory misapplications.
- Outcomes and Appeals: Reported overturn rates ranged from 70–100%; however, repeated denials were observed in later rounds, often without recognition of successful appeals. Educational sessions were frequently deemed inadequate, with limited actionable guidance. Following the public health emergency, there was increased audit activity, particularly regarding stays exceeding 180 days, causing concern for dementia patient access.
- Recommendations: The survey proposed standardizing audit processes, limiting overlap, considering post-appeal error rates for targeting, and employing auditors with hospice expertise.
In broader context, CMS’s FY2024 Program Integrity Report attributes $26.3 billion in savings to TPE reviews and education, though hospice-specific data is unavailable. TPE-driven denials facilitate recoveries, but appeals remain prevalent due to inconsistent contractor practices. Trends indicate ongoing attention to general inpatient care and certifications amid fraud concerns, with no hospice-specific data yet published for 2025.
Providers seeking detailed results should consult their respective MAC portals (e.g., Palmetto GBA for Jurisdiction M). Hospices facing TPE audits are encouraged to utilize CMS resources, appeal denials, and apply educational guidance to minimize future errors.
This data highlights the educational intent behind TPE but demonstrates notable challenges in its application to hospice settings. For CERT reports, visit cms.gov/cert. For further details on specific denial codes or audit preparation, assistance is available.
Duplicate Claims
A common reason for claim rejection is the submission of duplicate claims. Providers may inadvertently send duplicates due to oversights or may resubmit if they believe a claim was lost or not processed. Additionally, corrections to omitted information can lead to resubmissions, resulting in rejections. Andrea Freibauer, provider outreach and education consultant for NGS, advises adjusting claims post-adjudication instead.
Medicare’s automated processing systems efficiently identify such errors, typically without manual intervention. According to Freibauer at the NHPCO conference, the system flags identical claims—those sharing codes and service dates—as duplicates and rejects them automatically.
Readers that are interested in hospice regulations and in particular, fraud and claims related issues can find numerous posts on this site, including a three-part series I did earlier this year. Part III is available here and Parts I and II are linked at the top of the post: Medicare Hospice and Home Health Fraud, Part 3 – Reg’s Blog