Last week, the U.S. Department of Health and Human Services Office of the Inspector General (OIG), issued a report regarding the performance of contracted state agencies with respect to nursing home (SNF) compliance surveys. CMS contracts with state agencies, typically state departments of health or divisions thereto, to perform compliance/regulatory activities (surveys) in nursing homes. The report is available here: OIG Report on Survey Performance
Per the report, “States’ responsibilities under the 1864 Agreements with CMS include conducting standard surveys for each nursing home at least once every 15 months to certify compliance (or noncompliance) with requirements for participation in Medicare and Medicaid. (CMS uses 15.9 months to evaluate whether States meet this requirement.) Additionally, States conduct complaint surveys (abbreviated surveys used to investigate allegations of noncompliance) to investigate complaints about nursing homes, which is a critical safeguard to protect vulnerable residents.”
During the pandemic, CMS suspended regular survey activities as detailed above, concentrating primarily on infection control surveys based on reported outbreak data and potentially serious complaints involving resident injury, abuse, etc.
What OIG did as generation for this report is to look at CMS’ oversight of survey activities within the states across a timeframe from 10/2015 to 10/2018 (government fiscal years). Interviews were conducted with central office staff (Maryland) and regional staff (10 regions) regarding interactions with state survey agencies and how the staff worked with state regulators on survey performance problems (timeliness, follow-through, resurveys on citations, etc.). OIG also looked at records from states with poor performance history regarding the imposition of remedies and sanctions (fines, etc.).
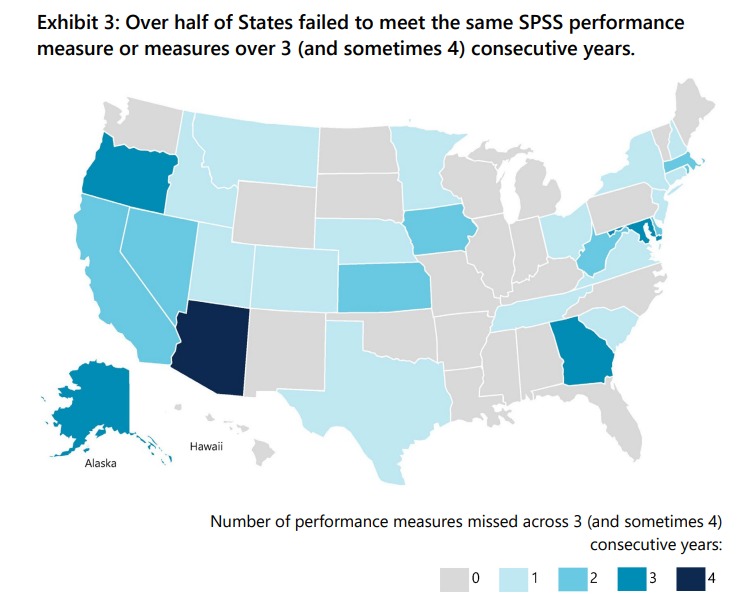
What OIG found was that a little more than half of States (28) failed to meet a performance measure or measures in 3 or 4 consecutive years during FYs 2015–2018. The most frequently missed performance measures involved survey timeliness, primarily attributed to staffing shortages. CMS imposed remedies on the states missing performance measures, requiring them to submit corrective action plans. Within the states where remedies were required, 10 percent were missing from CMS files and others lacked remediation detail.
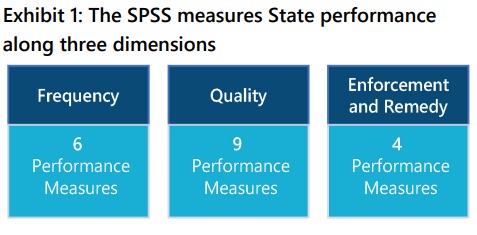
CMS uses a Performance Standards System to analyze state agency performance within its nursing home survey and certification activities. The regional (CMS) offices use the SSPS (system) to evaluate how States are meeting the survey performance requirements and to identify areas where state agencies need to improve the supervision/oversight of their survey and certification tasks. The SPSS sets measures and thresholds that are minimum scores for meeting the performance measures. CMS considers performance to be “inadequate” when agencies do not meet a set performance threshold.
When states fail to meet various performance standards, CMS can impose remedies on the state agency and state, including withholding of payments/funding to the agencies (rare). The remedies CMS can impose are found in the State Operations Manual (the regulatory manual for survey and certification activities in nursing homes).
Although most remedies are imposed at the discretion of the CMS regional offices, CMS does require states, for each performance measure that is not met, to file a corrective action plan. (For FY 2018, CMS did not always require States to develop corrective action plans for 2 of the 12 performance measures if the failure was due to implementation of the new survey process.)
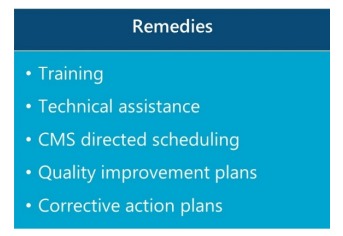
Once remedies are imposed, a state that demonstrates consistent performance issues (non-compliance), can be subject to sanctions. Sanctions, however, are rare as CMS’ own monitoring of agency activity is slow and often non-responsive in its own right.

Addressing the survey performance gaps is a challenge for CMS. First, funding for audits and survey activity has not kept up with the increase in regulatory requirements. Surveys take time and resources, principally manpower. A Senate Special Committee on Aging report confirms that 32 state survey agencies have vacancy rates (0pen positions) 20% or higher. (I’ll cover this report in detail in a future post). As staff shortages impact survey activity, states are turning to contractors to fill duty gaps. Contractors come at a cost, often higher than the compensation related costs to the employed staff that would typically fill the vacancies (if such staff were available).
To improve survey performance, OIG is recommending the following steps be taken on the part of CMS.
- Actively monitor states’ corrective action plans.
- Establish guidelines for progressive enforcement actions.
- Engage with senior state officials earlier and more frequently to address problems.
- Revise the State Operations Manual to reflect current CMS oversight practices.
- Disseminate the results of state performance reviews more widely.
I have advocated for decades that the survey and certification system is beyond repair and should be overhauled or better, abandoned as a task delegated to the states. SNFs/nursing homes should be treated the same as hospitals, home health agencies, hospices, etc., whereby deemed status accreditation is employed. Using an accreditation agency such as Joint Commission would give SNFs a quality outcome -based/quality improvement focused survey not a survey focused on paper compliance. CMS should focus then on poor performing facilities, allowing resources to go toward quicker removal from certification or, quicker return to compliance. Good facilities, consistently high performing, should have a three-year window for review.
Even bigger gains in quality and compliance could be made if CMS were to undertake a full-scale revamp of the Conditions of Participation, focusing far less on paperwork (MDS, etc.) and documentation requirements and staffing mandates (known to have near zero impact on quality) and more on outcomes and process improvement.