Medicare home health and hospice billing fraud has emerged as a significant issue within the U.S. healthcare system, costing taxpayers billions of dollars annually and jeopardizing the integrity of federal health programs. Fraudulent practices in this sector not only drain public resources but also compromise the quality of care provided to vulnerable populations, including the elderly and terminally ill. The Centers for Medicare & Medicaid Services (CMS) and the Department of Justice (DOJ) have intensified their efforts to combat these fraudulent activities, which range from billing for unnecessary or non-existent services to illegal kickback schemes. About 1.7 million Medicare beneficiaries receive hospice care each year, and Medicare pays about $23 billion annually for this care.
Recent cases highlight the pervasive nature of this problem. For example, private equity-owned Gentiva, formerly Kindred at Home, agreed to pay $19.4 million to settle allegations of billing Medicare and Medicaid for hospice services provided to patients who were not terminally ill, as well as paying kickbacks to induce referrals. Similarly, Strauss Ventures LLC, operating as The Grand Health Care System, paid $21.3 million to resolve claims of submitting false Medicaid claims for therapy services that were deemed unnecessary or never provided.
The financial impact of such fraud is staggering. CMS estimates that improper or fraudulent payments in the home health care sector alone accounted for more than $10 billion annually, representing over half of the total reimbursements in some year. Fraudulent hospice claims also contribute significantly to this issue, with regulators reporting that nearly one-third of general inpatient hospice stays in 2012 were billed inappropriately, costing Medicare $268 million (Hospices Inappropriately Billed Medicare Over $250 Million for General Inpatient Care (OEI-02-10-00491; 03/16).
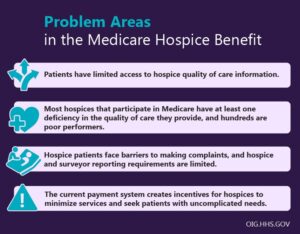
The consequences of these fraudulent activities extend beyond financial losses. Fraudulent billing practices can lead to inaccurate medical records, delayed or denied care for patients, and strained resources for legitimate providers. Moreover, these activities hinder CMS’s ability to justify reimbursement rate increases, potentially impacting the sustainability of care for underserved communities.
This post and following posts (a three-part series), delve into the scope, methods, and consequences of Medicare home health and hospice billing fraud, as well as the regulatory measures and legal actions being taken to address this pervasive issue. By examining recent cases and enforcement trends, this post aims to shed light on the systemic challenges and propose strategies to mitigate fraud in this critical sector of healthcare. More background is here: https://rhislop3.com/hospice-fraud-and-abuse-front-and-center/
Table of Contents
Medicare Home Health and Hospice Billing Fraud: An Overview
- Patterns of Fraudulent Activity in Home Health Billing
- Geographic Hotspots for Fraudulent Practices
- Common Fraudulent Practices in Hospice Billing
- Financial Impact of Medicare Fraud in Home Health and Hospice
- Regulatory and Enforcement Efforts
Recent Cases and Settlements in Medicare Fraud
- High-Profile Hospice Fraud Convictions
- Settlements Under the False Claims Act
- Intrepid USA Settlement
- Guardian Hospice Case
- Intrepid USA Settlement
- Fraudulent Practices in Telemedicine and Laboratory Services
- Fraudulent Hospice Practices Targeting Vulnerable Populations
- Enforcement Trends and Legal Implications
- Increased DOJ and HHS-OIG Collaboration
- Criminal and Financial Penalties
- Role of Whistleblowers
- Emerging Patterns and Future Challenges
- Expansion of Fraudulent Schemes
- Regulatory and Technological Responses
- Ethical and Social Implications
Impact and Regulatory Measures Against Fraudulent Practices in Medicare Home Health and Hospice Billing
- Strengthened Provider Enrollment Processes
- Data Analytics and Predictive Modeling in Fraud Detection
- Legislative Actions and Policy Reforms
- Enhanced Collaboration Between Agencies
- Public Awareness and Whistleblower Protections
- Targeted Oversight of Geographic Hotspots
- Future Directions in Combating Medicare Fraud
In part 2, I’ll cover the overview elements of fraud and data on recent cases (outline above). Next post will be early next week!