On December 29, 2025, the Centers for Medicare & Medicaid Services (CMS) announced the inaugural state awards from the $50 billion Rural Health Transformation Program CMS Announces $50 Billion in Awards to Strengthen Rural Health in All 50 States | CMS. The program was created as a policy vehicle to mitigate the potential negative effects of Medicaid premium subsidy lapses and resulting premium increases for ACA (Obama Care) plans. Full program background follows as well as an update on where initial grants awards stand.
Purpose and Funding of the Program
The Rural Health Transformation Program (“the Program”) was instituted to alleviate the effects of Medicaid cuts under OBBB. It will provide states with $10 billion annually for each fiscal year from 2026 through 2030, totaling $50 billion over five years. The District of Columbia and U.S. territories are not eligible participants in this Program.
Each year, 50% of Program funds will be distributed equally among the 50 states. The Centers for Medicare and Medicaid Services (CMS) has broad authority over the allocation of the remaining 50% of funds annually. States are permitted to use Program funds received for a given fiscal year until the conclusion of the subsequent fiscal year.
Application Process and Reporting Requirements
States must submit an application to receive Program funds. The specified “application submission period” concludes no later than December 31, 2025. CMS is required to approve or deny all applications by this date, implying that the application deadline will precede December 31 to allow sufficient time for review and processing.
States awarded Program funds must file annual reports with CMS detailing expenditure. Should a state misuse the allocated funds, CMS reserves the right to recoup those resources.
Allotments
Program allotments are available exclusively to states with approved applications. For the purposes of this document, it is assumed that all 50 states will apply for and receive approval for 2026 funds. Upon approval of a state’s 2026 application, there are no further application requirements for subsequent years under the Program.
Distribution of Funds
From 2026 to 2030, 50% of Program funds ($5 billion per year) will be divided equally among the 50 states, resulting in approximately $100 million per state per year. The remaining 50% constitutes “Tier 2 funds.”
CMS Discretion and Criteria for Tier 2 Funds
CMS retains significant discretion in disbursing Tier 2 funds. Program guidelines stipulate that at least one-quarter of states must receive Tier 2 allocations, meaning all such funds could be directed to as few as 13 states, while up to 37 may receive none. Nonetheless, excluding a substantial number of states may present political challenges.
In making Tier 2 allocations, CMS must consider three objective criteria:
- The proportion of the state’s population residing in rural census tracts within metropolitan statistical areas;
- The relative share of rural health facilities in a state compared to the national total;
- The status and circumstances facing hospitals within the state.
Additionally, CMS may weigh any other factors deemed appropriate.
Definition of Rural Health Facility
One of the objective criteria for awarding Tier 2 funds pertains to the quantity of rural health facilities within a state. The Program defines a “health care facility” as an entity that is (1) located in a rural area; (2) classified as rural; or (3) situated within a rural census tract of a metropolitan statistical area.
A “rural health facility” encompasses:
- Critical access hospitals (CAHs)
- Sole community hospitals
- Medicare-dependent, small rural hospitals
- Low-volume hospitals (LVHs)
- Rural emergency hospitals (REHs)
- Rural health clinics
- Federally qualified health centers (FQHCs)
- Community mental health centers
- Opioid treatment programs
- Health centers funded under section 330 of the Public Health Service Act
- Certified community behavioral health clinics located in a rural census tract
It should be noted that FQHCs, community mental health centers, and section 330 grantees are not exclusively rural entities, as their locations may include urban or suburban regions.

Requirements for a State Rural Health Transformation Plan
To join the Program, states must submit a detailed rural health transformation plan. However, this plan does not determine how funds are spent; instead, there are separate requirements and an additional plan for fund usage.
A key issue is how the eight required transformation plan components relate to the ten fund-use categories. CMS may require spending to match specific components or merge allowable uses into one list. More guidance from CMS is pending, but currently, CMS seems focused on ensuring appropriations adhere to the use-of-funds categories as outlined by statute.
Components of the Rural Health Transformation Plan
- Strengthen access to hospitals and other health care providers for rural populations.
- Improve health outcomes among rural residents.
- Promote adoption of innovative technologies, particularly for chronic disease prevention and management.
- Establish and enhance strategic partnerships between rural hospitals and other local or regional providers to support quality improvement, financial sustainability, and dissemination of best practices.
- Advance economic opportunity and increase the supply of health care professionals through targeted recruitment and training initiatives.
- Support data-driven and technology-enabled solutions that facilitate high-quality care delivery in proximity to patients’ homes.
- Develop measures to ensure long-term financial stability and sustainable operating models for rural hospitals.
- Evaluate factors contributing to increased risk of closure, service reduction, or conversion among independent rural hospitals.
Requirements for Use of Funds
States must allocate Program funds to at least three out of ten specified use-of-funds categories:
- Implementing evidence-based interventions to improve prevention and management of chronic diseases.
- Making payments to health care providers for medical items or services.
- Supporting consumer-focused, technology-driven solutions aimed at chronic disease prevention and management.
- Funding training and implementation support for technology adoption in rural hospitals, including tools such as remote patient monitoring, artificial intelligence (AI), or robotics.
- Recruiting and retaining clinical workforce professionals in rural areas for a minimum of five years.
- Enhancing information technology infrastructure to strengthen cybersecurity and optimize patient outcomes or operational efficiency.
- Assisting rural communities in optimizing their health care delivery systems.
- Facilitating access to treatment for opioid use disorder and mental health conditions.
- Fostering the development of innovative care models, such as value-based arrangements or alternative payment structures.
- Supporting additional initiatives designed to maintain access to high-quality health care services.
Rural Health Transformation Program: State Awards and Funding Structure
On December 29, 2025, the Centers for Medicare & Medicaid Services (CMS) announced the inaugural state awards from the $50 billion Rural Health Transformation Program, commonly referred to as the “rural health fund.” This initiative is overseen by the newly formed Office of Rural Health Transformation.
All fifty states submitted applications to participate in the rural health fund and each received an award. CMS will distribute $10 billion annually from fiscal year 2026 through 2030, with disbursements beginning in 2026.
Distribution of State Awards
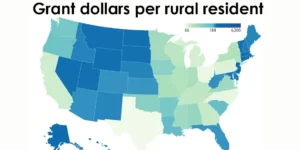
In 2026, the average state award is $200 million, ranging from $147 million for New Jersey to $281 million for Texas. While Texas has a much larger rural population than New Jersey, its funding is only about double due to statutory rules: 50% of the fund is divided equally among approved states ($100 million each per year through 2030), regardless of need. As a result, first-year awards per rural resident vary widely—from under $100 in ten states to over $500 in eight (see Figure 2). Texas receives the lowest per-rural-resident amount ($66), while Rhode Island, New Jersey, and Alaska see much higher rates. Only 25% of the $50 billion fund is allocated based on need, and just 5% directly reflects rural population size, with other factors like facility count and hospital DSH status considered.
Program Funding Distribution and Stakeholder Concerns
The Rural Health Transformation Program distributes $10 billion annually, splitting funds equally among states and allocating the rest based on factors like rural population, land area, facility needs, and policy proposals. States must report to CMS each year, but funding isn’t tied to performance or directly required to support rural hospitals. This has raised concerns that resources may be diverted to administrative projects instead of urgent rural provider needs. For more detail on the state of rural hospitals and their finances, see my post here: https://rhislop3.com/rural-healthcare-still-struggling/
Some states use these funds for long-term investments in care models, workforce development, and data systems rather than immediate financial relief. While this approach is strategic, rural hospitals with limited cash reserves fear they may struggle to benefit. With many states awaiting federal approval for their plans, hospitals remain uncertain about timelines and eligibility. As a result, they are cautiously preparing proposals, seeking partnerships, and advocating for more direct funding, knowing final decisions lie with state agencies.