The U.S. Department of Justice (DOJ) filed a False Claims Act lawsuit on April 4, 2025, against Vohra Wound Physicians Management LLC, Dr. Ameet Vohra, and VHS Holdings, P.A., in the U.S. District Court for the Southern District of Florida (Case No. 25-cv-21570). The complaint alleges that since December 2017, Vohra engaged in a nationwide scheme to defraud Medicare by submitting thousands of false claims for surgical debridement procedures, resulting in millions in improper reimbursements. The allegations center on three tactics:
- Proprietary EMR Software: Vohra’s Electronic Medical Record system allegedly auto-coded debridements as surgical (CPT 11042–11047), even when they were nonsurgical or not performed, and improperly applied Modifier 25 to bill for non-separately billable exams.
- Inadequate Physician Training: Vohra hired physicians without wound care experience, provided training that blurred surgical and nonsurgical debridement definitions, and omitted Medicare billing rules, leading to miscoded claims.
- Revenue-Driven Targets: Vohra set debridement quotas based on revenue goals, pressuring physicians to perform or document unnecessary procedures, with metrics like “Revenue Per Encounter” and threats of termination.
The DOJ claims this led to upcoding and billing for medically unnecessary services, violating Medicare’s global surgical package rules. The case is handled by the DOJ’s Civil Division, U.S. Attorney’s Offices for the Southern District of Florida and Georgia, and the HHS Office of Inspector General. The DOJ press release is here: Office of Public Affairs | United States Files False Claims Act Complaint Against Vohra Wound Physicians Management and Its Owner Alleging False Claims for Wound Care Services | United States Department of Justice
Vohra responded on April 7, 2025, denying the allegations, asserting that the case hinges on ambiguous Medicare billing codes and differing treatment philosophies (managing vs. actively healing wounds). They claim their EMR system is misrepresented, their physicians exercised independent judgment, and their approach is supported by clinical data showing effective wound healing. Vohra has engaged with the government since a 2018 subpoena, sought Medicare guidance, and is open to an amicable resolution but prepared to defend itself in court. Vohra Wound Physicians Responds to Department of Justice Lawsuit
Defense Perspective: Vohra may argue the EMR was an efficiency tool, not a fraud mechanism, and that ambiguous Medicare rules led to good-faith errors, not knowing violations (a key FCA element). Proving “scienter” (intent) could be a hurdle for the government.
Per the complaint (available here vohra_complaint_as_filed ) “Vohra compensated its physicians on a fee-for-service basis based on a fee schedule established by Vohra WPM. The more Medicare paid for the service, and the more revenue the Vohra Companies received for the service, the higher the physician was paid for that service. For example, Vohra physicians were paid more for muscle or bone debridements than subcutaneous debridements.”
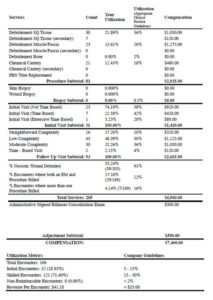
Various tools were used to monitor physician performance and to enforce expectations around the number of surgical wound treatments were provided. The tools tracked provider performance in terms of number of debridment procedures. Physicians that did not meet the expectations were subjected to additional training and could be ultimately, removed form VOHRA association.

As readers and followers will know, the allegations in the VOHRA case are the most common fraud/false claims allegation typically pursued – upcoding and payments tied to non-medically necessary services. A number of years ago, I wrote a fairly detailed post on the False Claims Act. It is available here: https://rhislop3.com/false-claims-act-providers-beware/