The Accreditation Commission for Health Care, Inc. (ACHC) has launched two new specialty credentials for organizations providing home care and/or hospice. These programs are in line with the Age-Friendly Health Systems (Care) programs and initiatives started by The John A. Hartford Foundation and the Institute for Healthcare Improvement (IHI), in partnership with the American Hospital Association (AHA) and the Catholic Health Association of the United States (CHA). Age-Friendly Health Systems | Institute for Healthcare Improvement (ihi.org)
According to the Age-Friendly program the US population aged 65 and over is projected to nearly double in the next 30 years, from 43.1 million in 2012 to an estimated 83.7 million by 2050. While these demographic changes are remarkable, they have outpaced our health systems, which are struggling to consistently deliver evidence-based care to every older adult at each point of care.
The ACHC accreditation initiative provides a Distinction in Age-Friendly Care for Home Health and Hospice, as well as a Distinction in Outcomes for Home Health, both aimed at acknowledging superior patient-centered care provided at home.
To receive the home health and hospice distinction, providers must proactively ensure patient safety and offer care that aligns with patients’ goals. Additionally, they must adopt the four evidence-based practices in geriatric care, referred to as the “4Ms”: What Matters, Medication, Mentation, and Mobility.
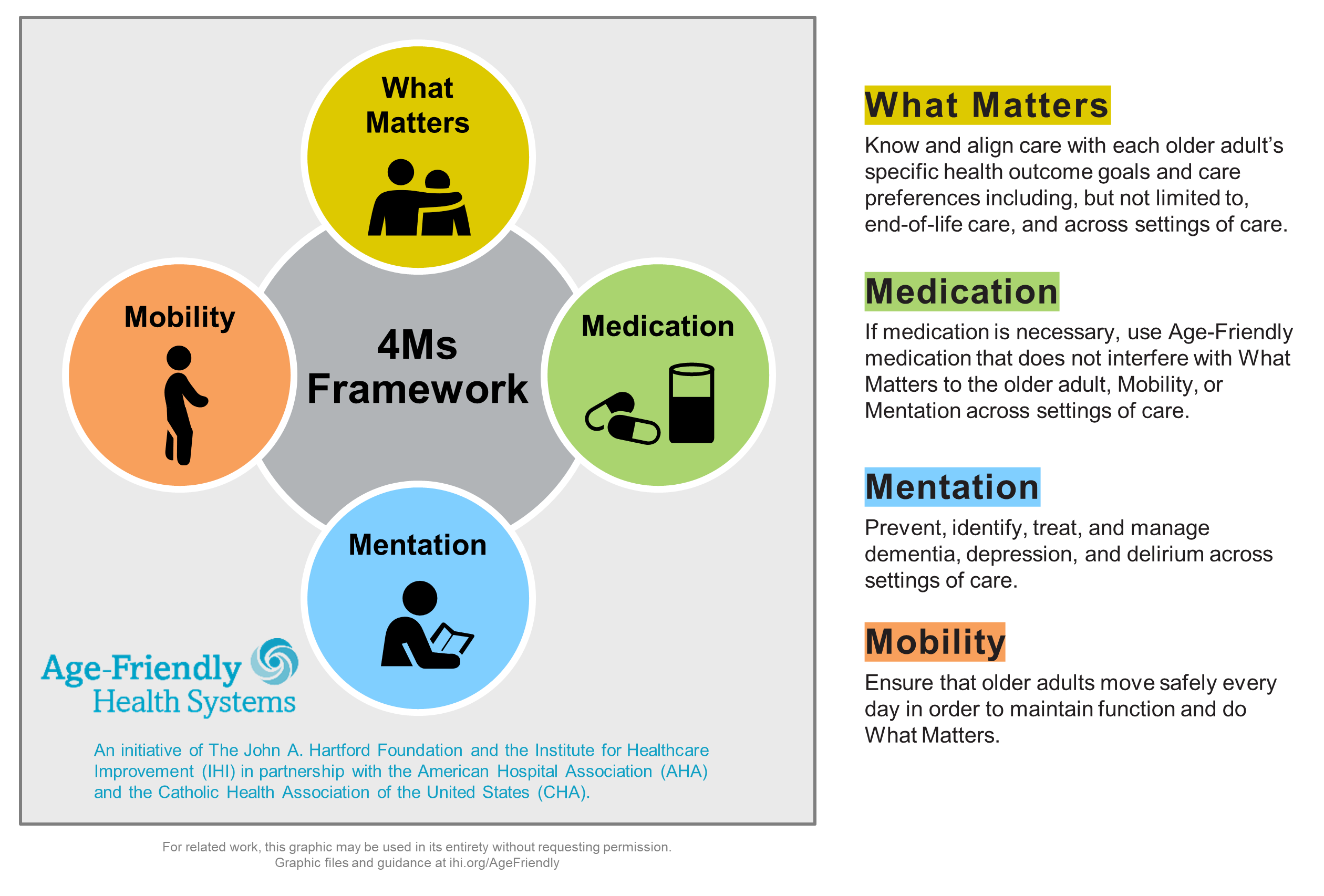
The 4Ms are central to the Age-Friendly Health Systems initiative due to the compelling evidence supporting their impact. When implemented collectively, they support and enhance each other. The 4Ms framework helps older adults and their healthcare providers communicate clearly with family and loved ones about priorities (What Matters); to prescribe Medications that do not interfere with those priorities, cognitive function (Mentation), or physical activity (Mobility); to proactively manage cognitive impairment (Mentation); and to promote daily physical activity (Mobility).
The Home Health Distinction in Outcomes aims to acknowledge exemplary performance across three key areas: patient outcomes, patient satisfaction, and healthcare utilization. These criteria are based on CMS’ Home Health Value-Based Purchasing Model, which evaluates providers against their peers using aggregated Medicare claims and additional data.
Any agency that scores in the top 25% of their provider cohort is eligible to receive the designation – Home Health Distinction.
The programs utilize a specialized geriatric assessment centered on the functional, psychosocial, and medical needs of elderly individuals. Agencies are required to prioritize medication management, addressing the polypharmacy risks that can adversely impact mobility and cognition, and to show efficient care coordination.
For most provider organizations, the question will be “is it worth it?” Typically, when program initiatives come with no direct reimbursement increase or economic reward, the general provider tendency is to stay-clear (no need to incur additional cost, etc.). Yet, in a value-based care migratory environment such as the trend now, there are reasons to dig deeper into the value proposition.
For example, where reimbursement is effectively fixed per day or per episode of care (home health), the goal is to be efficient and effective, thus keeping more of the fixed payment as “revenue” (over-providing care equals more expense). The Institute for Healthcare Improvement developed what I think is quite good, a Business Case for Becoming an Age-Friendly Health System. It is available here:
My reasons that I think providers should explore at least the framework of the Age-Friendly Health System are below. Likewise, there are lots of posts on this site pertaining to value-based care, care coordination, etc. All fundamentally, tie together the Age-Friendly concepts https://rhislop3.com/2023/11/28/value-based-care-what-it-is-and-how-it-can-work-for-post-acute-providers/
- Poor care costs money by being inefficient and providing more resources than necessary to produce a quality outcome. Additional tests, too many medications, too much staff at the wrong level, more therapy than necessary, etc.
- Poor care typically ties to poor outcomes. Poor outcomes = compliance risk. Compliance risk = litigation risk, survey risk with forfeitures (SNFs).
- Poor performance in VBP = reimbursement reductions. Providers that score below the applicable thresholds will have Medicare funds withheld from their reimbursement.
- Poor care = marketing and public relations risk such that referrals and premium patients (those with the best payment sources) are diverted to better rated providers. Poor care in a competitive market also limits system formation and participation choices, especially in light of evolving programs like TEAM – https://rhislop3.com/2024/08/20/team-model-and-post-acute-care/
- Poor care and ratings = less favorable credit profiles (higher cost debt, more stringent terms, lower borrowing limits). Similarly, risk-based programs such as liability insurance are positively or negatively impacted by quality ratings (premiums, carrier access/participation).