Seven hundred fifty-six rural hospitals in the United States are at risk of closure due to financial instability, with over 40% classified as being at immediate risk. These figures are derived from the Center for Healthcare Quality and Payment Reform’s latest analysis, which utilizes current cost reports submitted to CMS and verified through December 2025. The report distinguishes between two tiers of vulnerability: hospitals at risk of closure and those facing immediate risk. Rural_Hospitals_at_Risk_of_Closing (1)
On average, rural residents must travel twice as far—approximately 18 miles—to access medical care compared to their urban counterparts. With more than 700 rural hospitals at risk, including 300 at immediate risk, this distance is likely to increase, further impacting affected populations. Unlike urban communities, rural areas often depend on these facilities for both primary and emergency care; therefore, each hospital closure diminishes access to preventative and routine healthcare services. In February of last year, I wrote a similar article on the pressure rural healthcare was facing Rural Healthcare Under Intense Pressure – Reg’s Blog
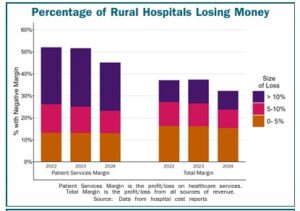
The predominant factor placing hundreds of rural hospitals at risk is inadequate reimbursement from private insurance plans, which often pay less than the actual cost of services provided. Medicare Advantage (MA) plans are included in this category. Historically, solutions have focused on increasing Medicare or Medicaid payments or expanding Medicaid eligibility, based on the misconception that most rural patients are covered by government programs or are uninsured. In reality, roughly half of all services provided at the average rural hospital are for patients with private insurance, including employer-sponsored and MA plans. Consequently, the payment rates set by private insurers more frequently determine a rural hospital’s financial viability.
Challenges Posed by Medicare Advantage
Medicare Advantage presents a complex, increasingly challenging environment for rural hospitals. While some studies indicate higher MA penetration might correlate with improved margins due to hospital characteristics, the American Hospital Association (The Growing Impact of Medicare Advantage on Rural Hospitals Across America | AHA ) and other experts emphasize the pressures stemming from lower MA reimbursements, administrative burdens such as prior authorization, delayed payments, and narrow networks. These challenges contribute to financial difficulties even when some analyses identify neutral effects.
- Lower Reimbursement: MA plans frequently reimburse at lower rates than traditional Medicare, reducing revenue for hospitals reliant on Medicare income.
- Administrative Burden: Strict utilization management policies add to operating costs and cause delays, particularly problematic for hospitals with limited staff.
- Payment Delays/Denials: Payment denials and delays strain the cash flow of rural facilities.
- Narrow Networks: Exclusion from MA networks can divert patient volume and revenue away from rural hospitals.
- Increasing MA Market Share: A growing proportion of Medicare revenue for rural hospitals now comes from MA, heightening exposure to these challenges.
Reasons for Closures
Multiple factors contribute to the ongoing wave of rural hospital closures, including declining patient volumes, low reimbursement rates from both public and private payers, staffing shortages, alternative care models, and additional operational challenges. Professor Alan Sager, an expert in health law, policy, and management, notes that accountability is lacking among governmental bodies and private insurers for addressing issues related to hospital need, capacity, service provision, and financial sustainability. No entity currently bears responsibility for ensuring adequate healthcare infrastructure and revenue to support necessary care delivery.
Despite this lack of accountability, Sager contends that affordable and accessible healthcare is achievable nationwide, citing the nation’s considerable healthcare expenditure—estimated at $5.6 trillion annually. He asserts that reform could be realized by curbing wasteful spending and ensuring adequate compensation for healthcare providers. Sager’s book, The Easiest, outlines a comprehensive plan for reform, noting that the U.S. spends significantly more per capita than other developed nations but achieves poorer outcomes.
All States have Closure Risk
Nearly every state has hospitals at risk of closure, with these facilities possessing financial reserves sufficient to cover losses for only six to seven years. In over half of all states, at least 25% of rural hospitals face this risk, and in ten states, 50% or more are jeopardized. Additionally, the report (see first paragraph) identifies 323 rural hospitals at immediate risk—meaning their financial reserves can sustain operations for no more than two to three years—a figure that has increased slightly in recent months.
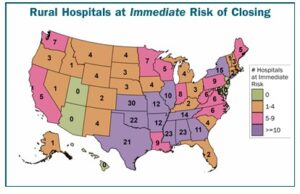
Below is a state-by-state listing of the number of rural hospitals at risk of closure in the next six to seven years and at immediate risk of closure over the next two to three years.
Alabama
28 hospitals at risk of closing (58%)
23 at immediate risk of closing in next 2-3 years (48%)
Alaska
3 hospitals at risk of closing (19%)
1 at immediate risk of closing in next 2-3 years (6%)
Arizona
4 hospitals at risk of closing (15%)
0 at immediate risk of closing in next 2-3 years (0%)
Arkansas
30 hospitals at risk of closing (64%)
12 at immediate risk of closing in next 2-3 years (26%)
California
18 hospitals at risk of closing (31%)
5 at immediate risk of closing in next 2-3 years (8%)
Colorado
11 hospitals at risk of closing (26%)
2 at immediate risk of closing in next 2-3 years (5%)
Connecticut
3 hospitals at risk of closing (75%)
2 at immediate risk of closing in next 2-3 years (50%)
Delaware
0 hospitals at risk of closing
0 at immediate risk of closing in next 2-3 years
Florida
8 hospitals at risk of closing (36%)
2 at immediate risk of closing in next 2-3 years (9%)
Georgia
22 hospitals at risk of closing (30%)
11 at immediate risk of closing in next 2-3 years (15%)
Hawaii
8 hospitals at risk of closing (62%)
0 at immediate risk of closing in next 2-3 years
Idaho
9 hospitals at risk of closing (33%)
1 at immediate risk of closing in next 2-3 years (4%)
Illinois
17 hospitals at risk of closing (22%)
10 at immediate risk of closing in next 2-3 years (13%)
Indiana
9 hospitals at risk of closing (16%)
8 at immediate risk of closing in next 2-3 years (15%)
Iowa
19 hospitals at risk of closing (20%)
4 at immediate risk of closing in next 2-3 years (4%)
Kansas
68 hospitals at risk of closing (68%)
30 at immediate risk of closing in next 2-3 years (30%)
Kentucky
17 hospitals at risk of closing (25%)
2 at immediate risk of closing in next 2-3 years (3%)
Louisiana
27 hospitals at risk of closing (48%)
9 at immediate risk of closing in next 2-3 years (16%)
Maine
11 hospitals at risk of closing (46%)
5 at immediate risk of closing in next 2-3 years (21%)
Maryland
0 hospitals at risk of closing
0 at immediate risk of closing in next 2-3 years
Massachusetts
2 hospitals at risk of closing (29%)
1 at immediate risk of closing in next 2-3 years (14%)
Michigan
10 hospitals at risk of closing (15%)
4 at immediate risk of closing in next 2-3 years (6%)
Minnesota
18 hospitals at risk of closing (19%)
7 at immediate risk of closing in next 2-3 years (7%)
Mississippi
36 hospitals at risk of closing (54%)
23 at immediate risk of closing in next 2-3 years (34%)
Missouri
29 hospitals at risk of closing (50%)
12 at immediate risk of closing in next 2-3 years (21%)
Montana
16 hospitals at risk of closing (30%)
4 at immediate risk of closing in next 2-3 years (8%)
Nebraska
7 hospitals at risk of closing (10%)
3 at immediate risk of closing in next 2-3 years (4%)
Nevada
5 hospitals at risk of closing (36%)
1 at immediate risk of closing in next 2-3 years (7%)
New Hampshire
4 hospitals at risk of closing (22%)
3 at immediate risk of closing in next 2-3 years (17%)
New Jersey
0 hospitals at risk of closing
0 at immediate risk of closing in next 2-3 years
New Mexico
8 hospitals at risk of closing (30%)
4 at immediate risk of closing in next 2-3 years (15%)
New York
24 hospitals at risk of closing (48%)
15 at immediate risk of closing in next 2-3 years (30%)
North Carolina
10 hospitals at risk of closing (18%)
6 at immediate risk of closing in next 2-3 years (11%)
North Dakota
13 hospitals at risk of closing (34%)
4 at immediate risk of closing in next 2-3 years (11%)
Ohio
7 hospitals at risk of closing (9%)
3 at immediate risk of closing in next 2-3 years (4%)
Oklahoma
48 hospitals at risk of closing (64%)
22 at immediate risk of closing in next 2-3 years (29%)
Oregon
7 hospitals at risk of closing (21%)
3 at immediate risk of closing in next 2-3 years (9%)
Pennsylvania
17 hospitals at risk of closing (33%)
9 at immediate risk of closing in next 2-3 years (17%)
Rhode Island
1 hospital at risk of closing (100%)
1 at immediate risk of closing in next 2-3 years (100%)
South Carolina
7 hospitals at risk of closing (32%)
4 at immediate risk of closing in next 2-3 years (18%)
South Dakota
9 hospitals at risk of closing (19%)
3 at immediate risk of closing in next 2-3 years (6%)
Tennessee
16 hospitals at risk of closing (31%)
14 at immediate risk of closing in next 2-3 years (27%)
Texas
82 hospitals at risk of closing (53%)
21 at immediate risk of closing in next 2-3 years (14%)
Utah
0 hospitals at risk of closing
0 at immediate risk of closing in next 2-3 years
Virginia
9 hospitals at risk of closing (29%)
6 at immediate risk of closing in next 2-3 years (19%)
Washington
19 hospitals at risk of closing (42%)
7 at immediate risk of closing in next 2-3 years (16%)
West Virginia
15 hospitals at risk of closing (44%)
6 at immediate risk of closing in next 2-3 years (18%)
Wisconsin
10 hospitals at risk of closing (12%)
5 at immediate risk of closing in next 2-3 years (6%)
Wyoming
7 hospitals at risk of closing (26%)
4 at immediate risk of closing in next 2-3 years (15%)